Intervensi Rutin di Dalam Persalinan

#gambar di ambil dari : http://www.bellybelly.com.au
Saya rasa semua wanita menginginkan proses persalinannya berjalan dengan lancar dan selamat. Dan saya yakin semua wanita menginginkan mendapatkan pengalaman yang menyenangkan saat melahirkan. Dan memang seharusnya demikian. Karena kita tahu bahwa melahirkanadalah proses yang tidak bakalan terlupakan oleh seorang ibu.
Kalau tak percaya….coba tanyakan kepada nenekmu, bagaimana proses kelahiran ibumu? Walaupun sudah puluhan tahun, sang nenek akan masih terus mengingat tentang proses persalinannya. Nah apa jadinya kalau proses persalinan menjadi proses yang traumatic? Pastinya nenek akan bercerita tentang traumana kepada Anda. Nah kalau udah demikian, bukankah itu justru menjadi semacam sugesti negative atau penularan rasa takut dan trauma kepada Anda? Dan ini akan mengakibatkan muncul trauma pada persalinan Anda juga?
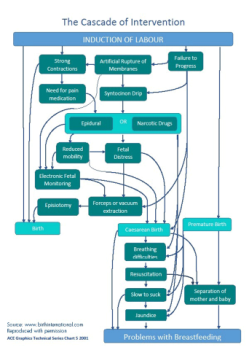
Nah salah satu langkah untuk menggapai persalinan yang nyaman dan minim trauma adalah dengan mencegah cascade intervensi.
Nah apa itu cascade intervensi dapat Anda simak di artikel saya sebelumnya di sini:
https://www.bidankita.com/cascade-intervensi-dalam-persalinan/
Nah itu bukan berarti semua intervensi punya efek negative lho ya? Namun paling tidak Anda harus menyadari dan mengerti mana intervensi yang perlu dilakukan, mana yang tidak dan mana yang bisa di hindari. Karena pada dasarnya semua intervensi dapat menyebabkan efek samping.
Nah saat ini saya akan membahas tentang intervensi rutin yang sering terjadi dalam proses persalinan:
Intervensi rutin umumnya dilihat sebagai suatu tindakan yang diperlukan untuk menjaga ibu dan bayi agar tetap aman selama proses kelahiran. Namun, Beberapa intervensi mungkin memiliki dampak negatif atau efek samping. Dan Mereka mungkin justru mengganggu proses fisiologi persalinan:
Contoh yang paling sering terjadi adalah Memisahkan ibu bersalin dari pasangannya, bayi atau keluarga dan teman yang menjadi pendampingnya.
Hal ini masih banyak terjadi dan dilakukan oleh beberapa tempat layanan kesehatan, dimana mereka melarang seorang ibu untuk di damping pasangan atau keluarga mereka saat melahirkan. Apa akibatnya?
- Ibu mendapatkan pengalamantidak nyaman dan tidak menyenangkan;
- Dapat mengakibatkan efek samping yang lebih serius lainnya
- Dapat menyebabkan penggunaan intervensi lainnya yang dirancang untuk memantau, mencegah atau mengobati efek samping ini (dikenal sebagai Cascade Intervensi).
Bukti ilmiah yang sekarang berkembang bahwa beberapa prosedur rutin ini berpotensi mengganggu atau menyebabkan kerusakan, dan bahkan malah tidak benar-benar bermanfaat bagi wanita atau bayi.
Nah apa saja intervensi rutin yang dapat menyebabkan bahaya dan tidak memiliki manfaat baik ibu atau bayi?
Penelitian menunjukkan bahwa bentuk-bentuk berikut perawatan atau prosedur meningkatkan risiko dan bisa jadi tidak memiliki manfaat untuk ibu dan bayi:
- Menawarkan dan melakukan pemeriksaan vagina selama persalinan secara berlebihan (link al.2013 Downe et).
- meningkatkan tekanan emosional (NICE 2007, Devane. 1996, Lewin et al. 2005).
- meningkatkan risiko infeksi pada bayi (Lumbiganon et al. 2004 Seaward et al. 1997 dan Hannah et al. 2000).
- Pemantauan denyut jantung bayi dengan doppler pada wanita berisiko rendah (Alfirevic et al. 2010 link).
USG doppler rutin tidak dianjurkan pada kehamilan berisiko rendah (NICE 2007: 35)
- Pemantauan janin elektronik terus menerus – monitor belt (. Alfirevic et al 2013 link).
- Lebih mungkin untuk mendapatkan intervensi obstetri kecil seperti analgesia epidural, pemantauan janin elektronik terus menerus berlangsung dan pengambilan sampel darah janin untuk gawat janin (Blix 2005);
- Meningkatkan risiko kelahiran dibantu vakum atau forsep (Alfirevic et al 2013.);
- meningkatkan risiko mengalami operasi caesar (Alfirevic et al 2013.);
- Berbaring selama persalinan atau kelahiran (Lawrence et al. 2013 link).
- meningkatkan durasi/lama persalinan (Lawrence et al.2013).
- meningkatkan risiko kelahiran caesar (Lawrence et al.2013).
- meningkatkan kebutuhan epidural (Lawrence et al.2013).
- meningkatkan risiko perdarahan yang signifikan (Terry dkk. 2006)
- meningkatkan risiko robekan perineum (Dudding et al. 2008)
- Meningkatkan risiko kerusakan otot dasar panggul (Fraser et al. 2000 Schaffer et al.2005, Handa et al.1996).
- Episiotomi untuk alasan apapun selain bayi yang tertekan (Dannecker Link et al. 2004)
- meningkatkan risiko kerusakan dasar panggul yang signifikan (Carroli dan Mignini 2009, DiPiazza et al. 2006, Gerdin et al. 2007, Altman et al.2007, Sartore dkk, 2004, Bick et al. 2008, Dannecker et al. 2004) .
- meningkatkan tekanan darah;
- meningkat resiko keidak nyamanan setelah melahirkan;
- meningkatkan risiko mual dan muntah;
- meningkatkan penggunaan obat untuk menghilangkan rasa sakit pada periode postnatal;
- meningkatkan jumlah perempuan kembali ke rumah sakit dengan pendarahan vagina (Begley di al. 2011).
Nah yuk tingatkan layanan bersalin dan pastikan bahwa intervensi rutin yang kita lakukan benar benar mempunyai bukti terbaik untuk ibu dan bayi
Anda bisa mulai belajar dari berbagai penelitian yang ada di sumber pustaka kami. Silahkan buka link nya satu persatu dan berdayakan diri Anda , demi buah hati.
- Albers, L. (1999) the duration of labour in healthy women. Journal of Perinatology. 19(2): 114-19.
- Alfirevic, Z., Devane, D., Gyte, G.M.L. (2013), Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Editorial Group: Cochrane Pregnancy and Childbirth Group. Published Online: 31 MAY 2013 available at http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006066.pub2/abstract [accessed on 15 November 2013].
- Altman, D., Ragnar, I. and Ekstrom, A. (2007). Anal sphincter lacerations and upright delivery postures: a risk analysis from a randomized controlled trial. International Urogynecology Journal, 18: 141-6.
- Begley CM, Gyte GML, Murphy DJ, et al. (2011) Active versus expectant management for women in the third stage of labour. Cochrane Database of Systematic Reviews, Issue 11. Chichester: John Wiley and Sons
- Bick, D., MacArthur, C. and Winter. H. (2008) Postnatal Care: Evidence and Guidelines for Management, 2nd edn. London: Churchill Livingstone.
- Blix, E., Reinar, L. and Klovning, A. and Oian, P. (2008) Prognostic value of the admission test and its effectiveness compared with auscultation only: a systematic review. BJOG, 112: 1595-604.
- Caldeyro-Barcia, R. (1979) Influence of maternal bearing down efforts during second stage on fetal well-being. Birth and Family Journal, 6(1): 7-13.
- Carroli, G. and Mignini, L. (2009) Episiotomy for vaginal birth. (Cochrane Review). In The Cochrane Library, Issue 1. Chichester: John Wiley & Sons, Ltd.
- Cesario, S. (2004) Re-evaluation of Freidman’s labour curve: a pilot study. Journal of Obstetrics, Gynecology and Neonatal Nursing, 33:713-22.
- Dannecker, C., Hillemanns, P. Strauss, A. et al. (2004) Episiotomy and perineal tears presumed to be imminent: randomised controlled trial. Acta Obstetrics et Gynecologica Scandinavia, 83: 364-8.
- Devane, D. (1996) Sexuality and Midwifery. British Journal of Midwifery, 4(8): 413-20.
- DiPiazza, D., Richter, H., Chapman, V., Cliver, S., Neely, C., Chen, C. and Burgio, K. (2006) Risk factors for anal sphincter tear in multiparas. Obstetrics and Gynecology, 107(6): 1233-6.
- Downe S, Gyte GM, Dahlen HG, Singata M. (2013). Routine vaginal examinations for assessing progress of labour to improve outcomes for women and babies at term. Cochrane Database Syst Rev. 2013 Jul 15;7:CD010088. doi: 10.1002/14651858.CD010088.pub2.
- Fraser, W., Marcoux, S., Krauss, I. et al. (2000) Multi-centre, randomised controlled trial of delayed pushing for nulliparous women in the second stage of labour with continuous epidural analgesia. American Journal of Obstetrics and Gynecology, 182: 1165-72.
- Gerdin E, Sverrisdottir G, et al. (2007). The role of maternal age and episiotomy in the risk of anal sphincter tears during childbirth. Aust N Z J Obstet Gynaecol 47 (4): 286-90.
- Handa, V., Harris, T. and Ostergard, D. (1996) Protecting the pelvic floor: obstetric management to prevent incontinence and pelvic organ collapse. Obstetric and Gynecology, 88: 470-8.
- Hannah M.E., Hannah, W.I., Hewson, S.A., et al. (2000) Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Lancet 2000; 256: 1375-83.
- Hodnett ED, Downe S, Walsh D. (2012). Alternative versus conventional institutional settings for birth. Cochrane Database of Systematic Reviews 2012, Issue 8. Art. No.: CD000012. DOI: 10.1002/14651858.CD000012.pub4.
- Johnstone, F., Aboelmagd, M. and Harouny, A. (1987) Maternal position in the second stage of labour and fetal acid base status. British Journal of Obstetrics and Gynaecology, 94(8): 753-7.
- Lavender, T., Hart, A., Smyth, R. (2013). Effect of partogram use on outcomes for women in spontaneous labour at term. Editorial Group: Cochrane Pregnancy and Childbirth Group. Published Online: 10 JUL 2013 at :http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005461.pub4/abstract . DOI:10.1002/14651858.CD005461.pub4
- Lawrence, A., Lewis, L., Hofmeyr, G.J., Styles, C. (2013). Maternal positions and mobility during first stage labour. Editorial Group:Cochrane Pregnancy and Childbirth Group. Available online at http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003934.pub4/abstract [Accessed on 1 April 2014]
- Lewin, D., Fearon, B., Hemmings, V., & Johnson, G. (2005). Women’s experiences of vaginal examination in labour. Midwifery, 21, 267-277.
- Lumbiganon, P., Thinkhamrop, J., Thinkhamrop, B., & Tolosa, J. E. (2004). Vaginal chlorhexidine during labour for preventing maternal and neonatal infections (excluding Group B Streptococcal and HIV). Cochrane Database of Systematic Reviews (4). The Cochrane Collaboration retrieved 17/04/09.
- NICE (2007) Intrapartum care: Care of healthy women and their babies during childbirth. Available online at http://www.nice.org.uk/nicemedia/pdf/IPCNICEguidance.pdf [accessed on 6 September 2013]
- Sandall, J., Soltani, H., Gates, S. et al (2013). Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database of Systematic Reviews, Issue 8. Available online at http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004667.pub3/abstract [accessed on 31 October 2013].
- Sartore, A., De Seta, F., Maso, G. et al. (2004) The effects of mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstetrics and Gynecology, 103: 669-73.
- Schaffer, J., Bloom, S., Casey, B. et al. (2005) A randomised trial of the effect of coached vs uncoached maternal pushing during the second stage of labor on postpartum pelvic floor structure and function. American Journal of Obstetrics and Gynecology, 192: 1692-6.
- Seaward PG, Hannah ME, Myhr TL, et al. International Multicentre Term Prelabor Rupture of Membranes Study: evaluation of predictors of clinical chorioamnionitis and postpartum fever in patients with prelabor rupture of membranes at term. American Journal of Obstetrics and Gynecology. 1997;177(5):1024–9.
- Smyth, M.D., Markham, C., Dowswell, T. (2013). Amniotomy for shortening spontaneous labour. Editorial Group: Cochrane Pregnancy and Childbirth Group. Published Online: 18 JUN 2013, available at http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006167.pub4/abstract [accessed on 15 November 2013]. DOI: 10.1002/14651858.CD006167.pub4.
- Walsh, Denis (2012) Evidence and Skills for Normal Labour and Birth – A Guide for Midwives. Second Edition. New York: Routledge.
- Walsh, T. (2009) Exploring the effects of hospital admission on contraction patterns and labour outcomes using women’s perception of events. Midwifery, 25: 242-52.
- Zhang, J., Troendle, J. and Yancey, M. (2002) Reassessing the labour curve. American Journal of Obstetrics and Gynecology, 187: 824-8.
Semoga Artikel ini bermanfaat
Salam Hangat
Bidan Kita





Touche. Sound arguments. Keep up the good spirit.
I am amazed with this website, really. I’m a fan.